Does a head injury from a motor vehicle accident cause psychological injury?
You or someone you love has been injured in a motor vehicle accident. After the initial cuts and bruises heal, you think they are on the mend, but something still seems “off”. Perhaps they are less focused, more distracted. Maybe they don’t want to see friends, go out, enjoy the things they used to do. They might even seem sleepy, or extremely busy but not actually getting things done the way they used to. “What is going on?”.
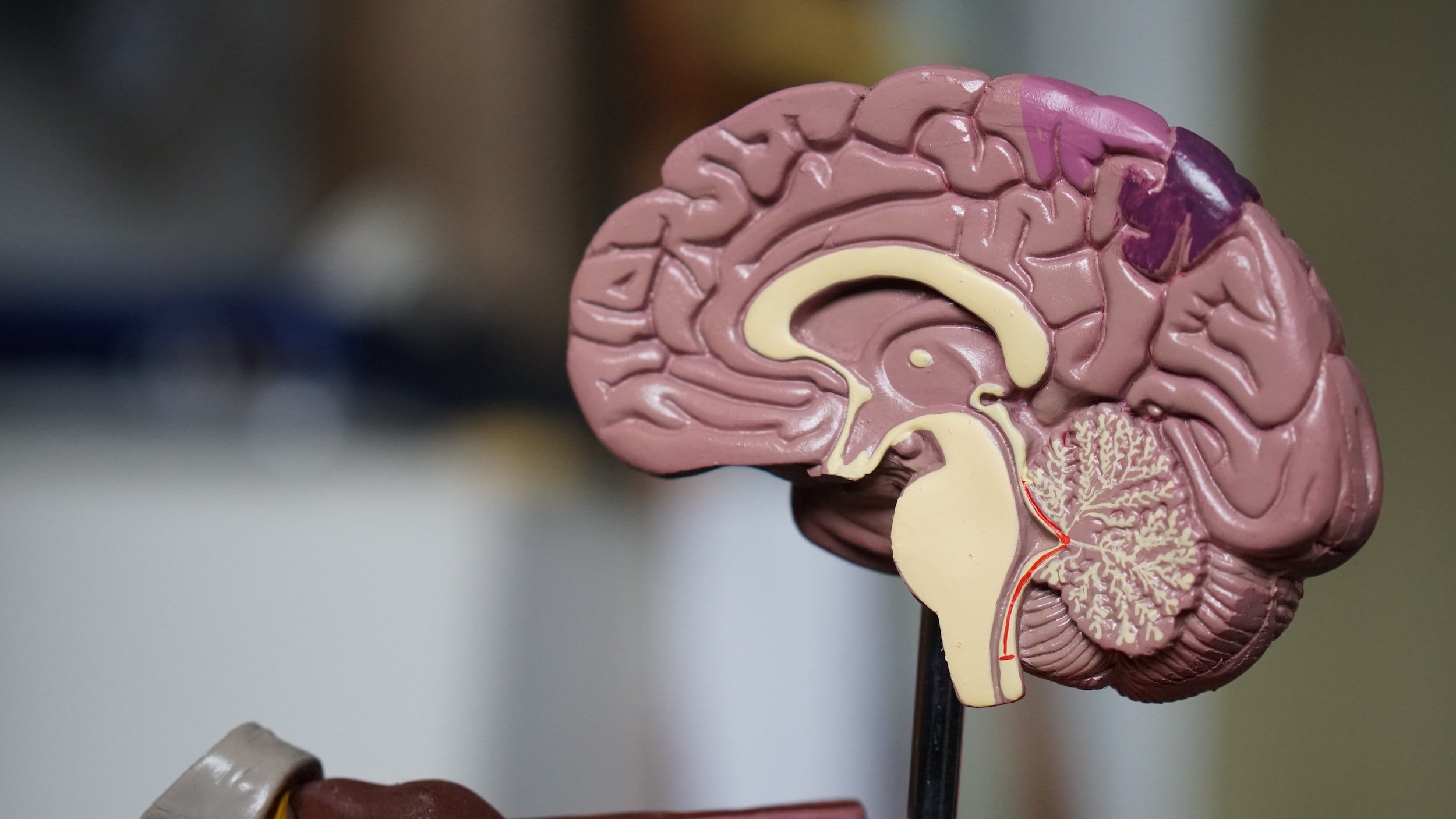
Motor vehicle accidents are the most common cause of brain injuries, accounting for about 40% of patients (Ontario Brain Injury Association 2012). Brain injuries are also a quite common consequence of motor vehicle accidents. The mechanism of these injuries can be either a direct impact to the head, or an injury caused by the rapid loss of speed during a car accident. Even if there is no impart directly to the head, the change in speed can cause the brain to impact against the inside of the skull. Because the injury can be either focused on one part of the brain, or widespread, and can be milder or more serious, there are many different effects which can be seen from traumatic brain injuries, or TBI. (Rao 2000)
Where the injury is direct, it can result in bruising and bleeding of the brain inside the skull. There can also be bleeding of the tissues between the brain and the skull, which puts pressure on the brain. When the brain is shifted or stretched within the skull, there can also be shearing and stretching of the axons. This injury, called a diffuse axonal injury, can have a whole list of additional consequences, not all of which are things one would normally associate with a head injury. (Brain Injury Society of Toronto n.d.)
Changes in behaviour can be a result of the injury itself, or a behavioural response to the stresses that result from the injury. Some of the most common forms of mood changes are: depression, anxiety, apathy, dyscontrol disorder, sleep disturbances, and headaches. (Rao 2000)
Depression was the first of the mood disorders to be associated with TBI, and it is also the most commonly reported. About 25% of TBI patients report suffering depression in the period 6 to 24 months after the original injury. Patients report feeling loss, fatigue, irritability, discouragement, and demoralization. The mechanism of the depression is probably related to the disruption of the of the basal ganglia, which is the part of the brain that controls emotions, executive functioning, and the flow of information between the various parts of the brain (Lanciego 2012). Whether these feelings are the result of the injury to the brain, or a reaction to the patient living with the sequalae of the injury such as insomnia and memory loss, the feelings are the same (Ontario Brain Injury Association 2012). The patient is suffering, and the depression makes it harder for them to feel any hope or positivity. Treatment is the same as for any other form of major depression which could be a combination of medication, treatment, and psychological therapy.
Another common psychological consequence of TBI is anxiety disorder. This includes generalized anxiety disorder, panic disorder, phobic disorders, post-traumatic stress disorder, and even obsessive-compulsive disorder. (Rao 2000) The patients feel a sense of worry and fear which is free-floating, not directly caused by or associated with a specific trigger. The most current theory is that the changes in the neurotransmitter chemicals within the brain are responsible for these changes. Treatment includes both behavioural and psychotherapy, as well as medication. Many patients experience improvement with short-term treatment, while others need longer courses of treatment in order to recover and return to their normal selves.
Apathy often occurs along with depression, but it can also occur in patients that do not experience depression. Apathy in this context refers to a group of feelings such as disinterest in and disengagement from their normal lives, lack of motivation, and a loss of emotional response. Although these feelings are also seen in patients with depression, apathy patients do not demonstrate the same sort of negative reactions and thought patterns, or cognitive deficits. There are several theories about this type of apathy and anhedonia. (Ontario Brain Injury Association 2012) It may be related to the same diffuse axonal injury discussed above, and it may also be caused by the stress on the brain of having to compensate for other deficits. In any case, anhedonia and apathy can occur either with depression, or separate and apart from it.
Behaviour dyscontrol disorder is a more accurate name for a constellation of symptoms, often called post-concussion syndrome, that affect many TBI patients, to varying degrees. These symptoms may be experienced after any degree of head injury, whether there was a formal diagnosis of concussion. Patients experience changes in their mood, thinking, and behaviour. These symptoms are attributed to widespread micro-level injuries to the neural networks in the brain. When these injuries occur in the frontal areas of the brain, they can affect executive functioning and behavioural control (Lanciego 2012). Most patients recover substantially in the 6 to 24 months following the injury, but as many as 15% are still experiencing symptoms two years and longer after the injury.
Additional changes often experienced by TBI patients are sleep disorders, and headaches, among other symptoms. These symptoms are bothersome in themselves but can also contribute to the stress on the brain that causes or exacerbates other symptoms. (Brain Injury Society of Toronto n.d.)
There are a few things that can be helpful to remember, whether you are personally experiencing these symptoms, or caring for a loved one who is:
These changes in mood and behaviour are part of the brain injury. There is no reason to be embarrassed or feel guilty about psychological symptoms, any more than physical symptoms of an injury.
If the injury is yours, the feeling that nothing will help is a symptom of depression. There is hope, and there is help.
If it is happening to a loved one, changes from a brain injury do not change who the person is. The individual that you know and love is still there. Help them to access the help they need to get better.
There is treatment for the psychological symptoms of brain injury, and it can help. Make sure that you access the treatments that are most beneficial to your individual situation.
We at Singer Kwinter specialize in helping accident victims pursue their rights against their insurance company. Contact us for information about a free consultation with our lawyers.
Sources:
n.d. Brain Injury Society of Toronto. Accessed January 31, 2023. https://bist.ca/brain-injury-101.
Lanciego, J. L., Luquin, N., & Obeso, J. A. 2012. Functional neuroanatomy of the basal ganglia. Cold Spring Harbor perspectives in medicine, 2(12), a009621. Accessed February 6, 2023. https://doi.org/10.1101/cshperspect.a009621.
Ontario Brain Injury Association. 2012. "The OBIA Impact Report 2012: A Statistical Snapshot of Acquired brain Injury and its Effects on Survivors and Caregivers."
Rao, Vani and Lyketsos, Constantine. 2000. "Neuropsychiatric Sequelae of Traumatic Brain Injury." Psychosomatics, January-February.